Understanding and Managing Eczema: Skincare Tips for Relief
Eczema, often used to describe atopic dermatitis, is a chronic, relapsing skin condition marked by dryness, itch, and inflamed patches. While there’s no single cure, the right daily care can dramatically reduce flares, improve comfort, and protect your skin barrier. This guide explains what eczema is, common triggers, and practical skincare strategies you can start today.
What is eczema?
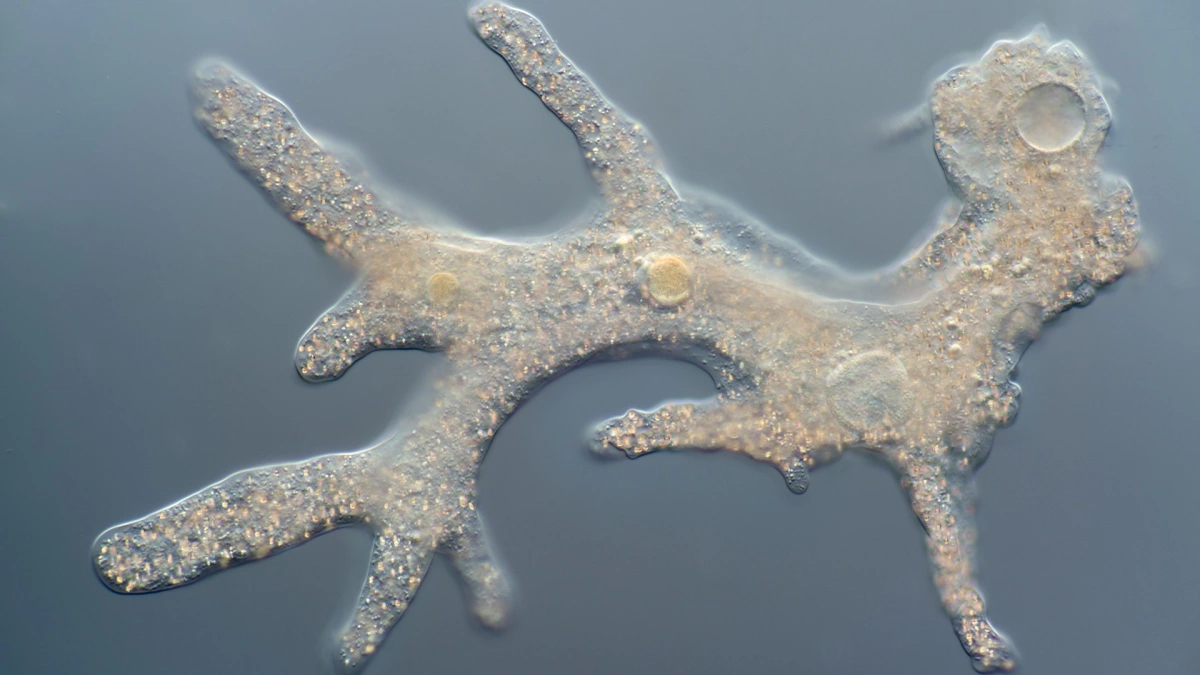
Eczema is an inflammatory skin condition that stems from a mix of genetic, immune, and environmental factors. A key issue is a weakened skin barrier: precious moisture escapes, irritants sneak in, and the immune system becomes overactive. Eczema often starts in childhood but can begin at any age. Flares come and go, and symptoms range from mild dryness to widespread, intensely itchy plaques.
How eczema looks and feels
- Dry, scaly, or rough patches
- Itch that worsens at night (scratching can thicken and darken skin over time)
- Redness on lighter complexions; purple, gray, or darker brown on deeper skin tones
- Small bumps that may ooze or crust during flares
- Post-inflammatory color changes after healing (darker or lighter spots)
Common sites include the face (especially in infants), neck, inside elbows, behind knees, hands, and ankles. On darker skin tones, eczema can be missed because it doesn’t always look red; pay attention to itch, texture, and color shifts.
Common triggers
- Dry air, cold weather, rapid temperature changes
- Hot showers, harsh soaps, frequent handwashing without moisturizing
- Fragrances, dyes, alcohol-heavy products, some essential oils
- Wool and rough fabrics; tight or sweaty clothing
- Stress, poor sleep
- Allergens such as dust mites, pet dander, pollens; occasionally certain foods
- Infections or skin injury from scratching
Not all triggers affect everyone; tracking your personal patterns is key.
Daily skincare routine
Morning
- Cleanse targeted areas with a gentle, fragrance-free cleanser if needed; otherwise rinse with lukewarm water.
- Apply your medication to active eczema patches as prescribed.
- Seal with a rich, fragrance-free moisturizer. For very dry skin, choose an ointment.
- Finish with broad-spectrum SPF 30+ on exposed skin. Choose mineral sunscreens (zinc oxide or titanium dioxide) if you’re sensitive.
Evening
- Short, lukewarm shower or bath (5–10 minutes). Pat skin dry—don’t rub.
- Within 3 minutes, apply any prescribed topical medication to affected areas.
- Immediately moisturize head to toe (“soak and seal”).
- Consider wet wraps during severe flares (see below) after discussing with your clinician.
Bathing and cleansing
- Temperature: use lukewarm water. Heat strips natural oils and worsens itch.
- Time: limit to 5–10 minutes once daily or every other day based on your skin’s needs.
- Cleanser: choose mild, fragrance-free, dye-free cleansers labeled for sensitive or eczema-prone skin. Avoid deodorant or antibacterial soaps unless advised.
- Technique: cleanse only where needed (folds, underarms, groin, feet); rinse well.
- Drying: gently pat with a soft towel, leaving a little dampness for better moisturizer absorption.
Moisturizing strategies
Moisturizers rebuild the barrier, reduce itch, and lengthen time between flares.
- Frequency: at least twice daily and after every wash; more often if hands are frequently washed.
- Type matters:
- Ointments (petrolatum, jelly-like): most occlusive and soothing; great for very dry skin and nighttime.
- Creams (thicker than lotions): good balance of hydration and comfort for daily use.
- Lotions (thinner): lighter feel but often less protective; may sting on cracked skin.
- “Soak and seal”: bathe, pat dry, quickly apply medication to lesions, then moisturize everywhere.
- Hands and feet: consider thicker ointments or overnight cotton gloves/socks after moisturizing.
Choosing products and ingredients
Look for short, simple ingredient lists. Patch-test new products on a small area for 2–3 days first.
Helpful ingredients
- Ceramides and lipids (restore barrier)
- Petrolatum, dimethicone, shea butter (occlusive and protective)
- Glycerin, hyaluronic acid (humectants that draw moisture in)
- Colloidal oatmeal, allantoin, panthenol (soothing)
- Urea or lactic acid (low strength) for rough, thickened areas if tolerated
Often best to avoid
- Fragrance (including essential oils) and masking perfumes
- Dyes and glitter
- Harsh alcohols, strong acids or retinoids on active eczema patches
- Lanolin if you’ve reacted before
Labels that say “fragrance-free” are preferable to “unscented.” Look for products vetted by eczema or allergy organizations when possible.
Managing flares
Flares still happen. Early, consistent treatment can shorten their duration.
- Topical steroids: often first-line for inflamed patches. Use the strength and duration prescribed by your clinician, usually as a thin layer once or twice daily for limited periods. Avoid prolonged use of high-potency steroids on the face, groin, or skin folds.
- Non-steroidal options: calcineurin inhibitors (tacrolimus, pimecrolimus) or topical JAK inhibitors may be used on sensitive areas or for maintenance—discuss suitability with your provider.
- Wet-wrap therapy: apply medication to active areas, then moisturizer to all skin; cover treated areas with a damp cotton layer and a dry layer on top for 2–8 hours or overnight. Useful for severe flares for a few days. Consult your clinician before combining with potent steroids.
- Infection watch: yellow crusts, pus, increasing pain, warmth, streaking, or fever warrant medical evaluation. Eczema herpeticum (sudden clusters of painful blisters or punched-out erosions) is urgent—seek care promptly.
- Phototherapy or systemic medications: for moderate-to-severe or refractory eczema under specialist care.
Relieving itch and protecting skin
- Keep nails short; consider cotton gloves at night.
- Use cool compresses for 5–10 minutes to calm hot, itchy areas before moisturizing.
- Moisturize instead of scratching; try gentle pressure or tapping as a substitute.
- Manage heat and sweat: take breaks to cool off; shower and moisturize after workouts.
- Sleep strategies: breathable bedding, room slightly cool, consistent schedule. Sedating antihistamines may aid sleep in some people; ask your clinician.
Clothing, laundry, and environment
- Fabrics: choose soft, breathable cotton or bamboo. Avoid rough wool or tight, scratchy garments.
- Laundry: use fragrance-free, dye-free detergents; skip fabric softeners or dryer sheets. Run an extra rinse cycle if sensitive.
- Humidity: aim for indoor humidity around 40–50%. A humidifier in dry seasons can help; clean it regularly to prevent mold.
- Temperature: keep rooms comfortably cool; sudden changes can trigger itch.
- Hand care: after washing or sanitizing, apply a barrier cream or ointment. Wear cotton liners under work gloves if needed.
Diet, stress, and lifestyle
- Stress management: mindfulness, breathing exercises, gentle yoga, or counseling can reduce flares linked to stress.
- Exercise: regular activity supports sleep and mood. Shower, rinse, and moisturize afterward to remove sweat and salt.
- Diet: no single eczema diet fits everyone. A balanced, anti-inflammatory pattern (fruits, vegetables, whole grains, lean proteins, healthy fats) supports overall skin health. Avoid unnecessary food restrictions—consider supervised testing if you suspect true food triggers.
- Alcohol and smoking: alcohol can worsen flushing; smoking harms skin healing. Reducing both may help.
- Allergen control: dust-mite covers for pillows/mattresses, frequent vacuuming with HEPA filtration, and pet-dander management may help if you’re sensitive.
Special situations
Infants and children
- Daily short baths and liberal moisturization are foundational.
- Use gentle, fragrance-free products; avoid bubble baths.
- Discuss any suspected food associations with a pediatric clinician before restricting diet.
Face and eyelids
- Prefer non-steroidal topicals or low-potency steroids short-term under guidance.
- Use bland moisturizers; mineral sunscreens are often better tolerated.
Hands
- Frequent moistening is essential. Carry a travel-size cream.
- For wet work or cleaning, wear protective gloves with cotton liners.
Darker skin tones
- Look for gray, purple, or darker brown patches and texture changes.
- Prevent and treat flares early to reduce post-inflammatory color changes.
- Use daily sunscreen to help minimize uneven pigmentation as skin heals.
Travel and seasons
- In cold, dry weather, switch to thicker creams/ointments and use a humidifier.
- In heat and humidity, prioritize sweat management, lightweight clothing, and frequent moisturizing after rinsing.
When to see a healthcare professional
- Flares are frequent, severe, or not improving with good skincare
- Skin shows signs of infection (pus, crusting, warmth, spreading redness, fever)
- Symptoms significantly affect sleep, school, work, or mood
- You have eye involvement, painful blisters, or sudden widespread rash
- You’re considering stronger treatments or are unsure how to use medications safely
This guide is educational and not a substitute for personalized medical advice. A clinician can tailor treatment, check for allergic contact dermatitis, and consider advanced therapies when needed.
Quick-start checklist
- Short, lukewarm showers; gentle cleanser only where needed
- Apply prescribed medication to active areas, then moisturize within 3 minutes
- Moisturize at least twice daily; use richer textures at night or for hands
- Choose fragrance-free, dye-free products; patch-test new items
- Wear soft, breathable fabrics; avoid wool and rough seams
- Use fragrance-free detergent; skip fabric softeners
- Keep room cool, humidity around 40–50%
- Manage stress, protect sleep, and rinse/moisturize after sweating
- Seek medical advice for persistent or complicated cases
With consistent care, most people can reduce flare frequency and feel more comfortable in their skin. Start with small, steady changes and build a routine that fits your life.